Hi and welcome back to part 2 of the series “Polymers in Ophthalmology”. This time, I’ll be talking about Lenses, Prostheses and other Medical Devices. If you missed part 1, you can find my post about Viscoelastic & Drug Delivery Formulations here.
Lenses
Let’s start with a popular ophthalmology product that everybody already knows – contact lenses. Contact lenses are mainly used to correct vision, but they also serve aesthetic purposes like changing your eye color, and can deliver drugs. Depending on the polymers used to manufacture the lenses, their properties can range from rigid glassy to soft hydrogels. However, most people buy soft contact lenses nowadays as they are more comfortable to wear.[1] The hydrogel lenses consist of either copolymers of hydroxy ethyl methacrylate (HEMA) and vinylpyrrolidone or are made of hydrophilic polysiloxane copolymers. The latter represent the newest development and feature enhanced oxygen permeability.
Contact lenses can also be impregnated with drugs. Researchers from China just reported a color-changing contact lens that delivers timolol, a common glaucoma drug. The lens was designed to change its color from green to blue during drug release to enable monitoring of the release rate.
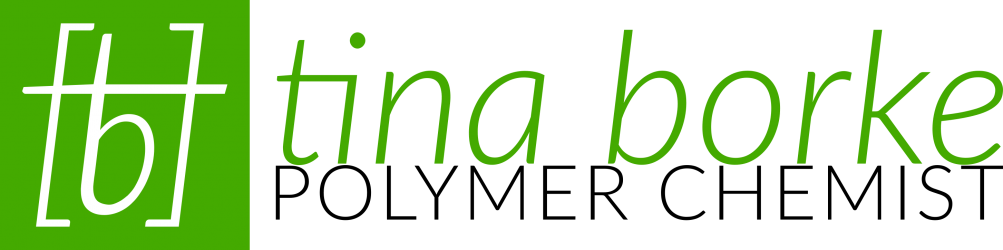
Intraocular lenses (IOLs) are frontrunners in the treatment of cataract, i.e. clouding of the natural lens. Cataract surgery is the second most frequently performed surgery in the European Union.[2] There the cloudy lens of the patient is removed and replaced with a clear polymer lens. The artificial lens should satisfy a range of desirable properties, such as being highly transparent and transmitting all visible light. High refractive index materials are favorable, because they can be fashioned into thinner lenses. Likewise, materials with a low Young’s modulus (meaning high elasticity) make foldable lenses, which can be implanted through a smaller incision in the eye. Commonly used polymers include hydrophilic or hydrophobic acrylate copolymers or polysiloxanes.[3] They also often contain UV-absorbing moieties or comonomers and are at least partially cross-linked.
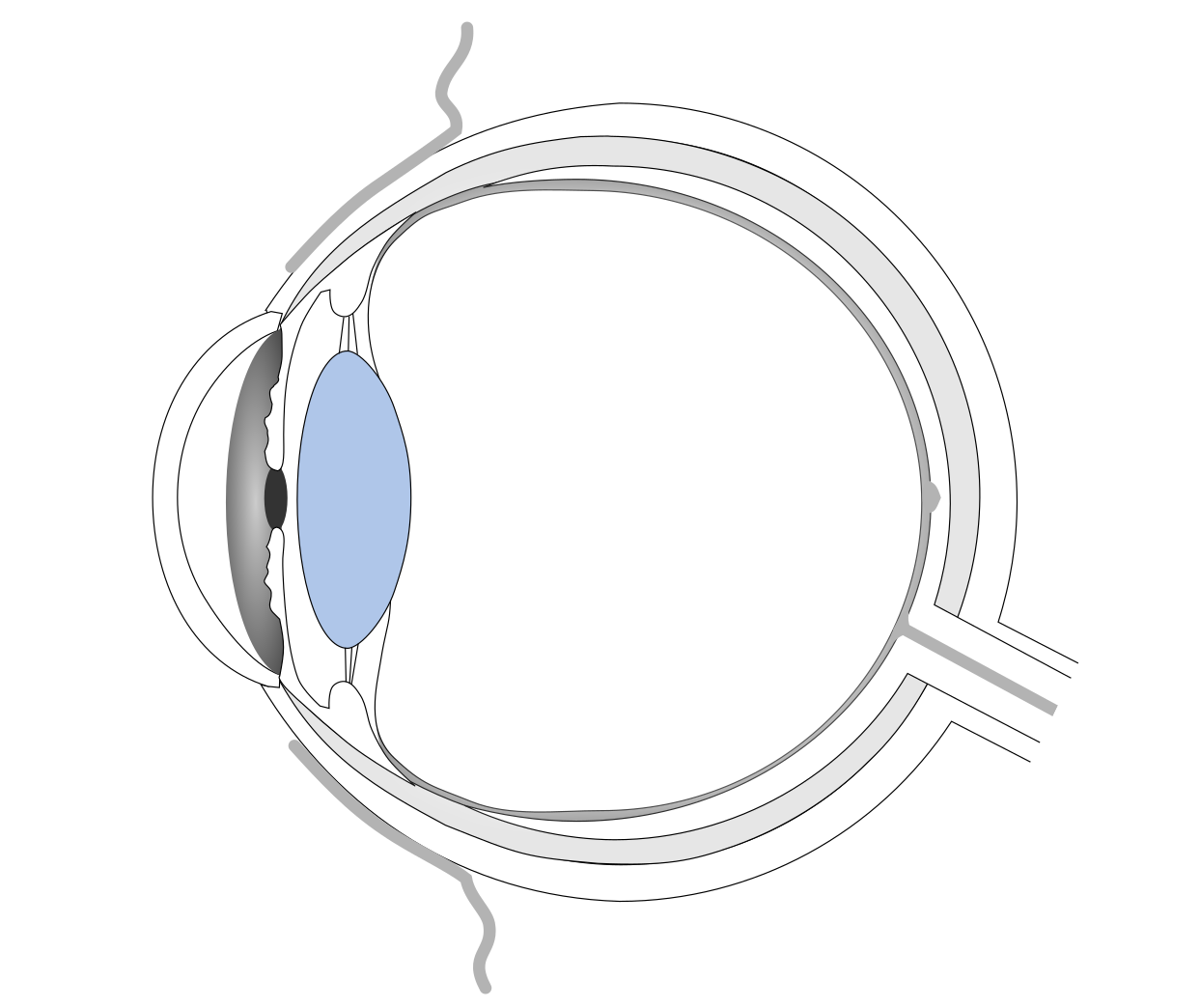
Phakic intraocular lenses are hybrids of contact lenses and IOLs. They have similar properties to IOLs, but are used to correct vision in people without cataract. The lenses are implanted in the anterior chamber of the eye, in front of the natural lens and are meant to stay there for good.[4]
Prostheses
Prostheses are replacements for different body parts and a range of polymer prostheses are available for the eye. For example, artificial corneas, also called keratoprostheses, can help patients with severely damaged corneas that have failed to receive donor transplants. The prostheses commonly consist of a transparent optical cylinder, surrounded by a porous ring that allows for penetration of cells into the material. In this way, tissue can grow into the prosthesis and anchor it onto the eye surface, while the middle part stays clear. The optical cylinder is usually made from polymethylmethacrylate (PMMA) and the porous ring can be PMMA or titanium.[5]
For patients with aniridia, a birth defect leading to absence of the iris, or injury-induced iris damages, there is as of this year one FDA-approved artificial iris (HumanOptics’ CustomFlex® ArtificialIris) on the market. Besides its cosmetic implications, absence of the iris also leads to light-sensitivity, glare effects and loss in depth of focus. The artificial iris from HumanOptics is hand-made from silicone polymer and pigmented to match the other eye. During implantation it is placed either in the lens capsular bag or between lens and ciliary body (in the so-called ciliary sulcus).
Another application for polymers in ophthalmology are artificial orbital walls. The orbit is the bone cavity that holds the eyeball. Injury-induced defects are often fixed with resorbable polymer plates made from polyesters (e.g. poly-lactic acid-co-glycolic acid or polycaprolactone), permanent plates of porous polyethylene, silicone sheets or Teflon implants (polytetrafluoroethylene).[6]
Ocular prostheses (artificial eyes) or “glass eyes” are, despite their name, frequently made of polymers, most notably PMMA. They can take the form of a whole eyeball in case of a missing natural eye, or a thin shell worn over a damaged eye. Did you ever notice that Peter Falk (aka Lieutenant Columbo) was wearing an artificial eye?[7]
Other Medical Devices
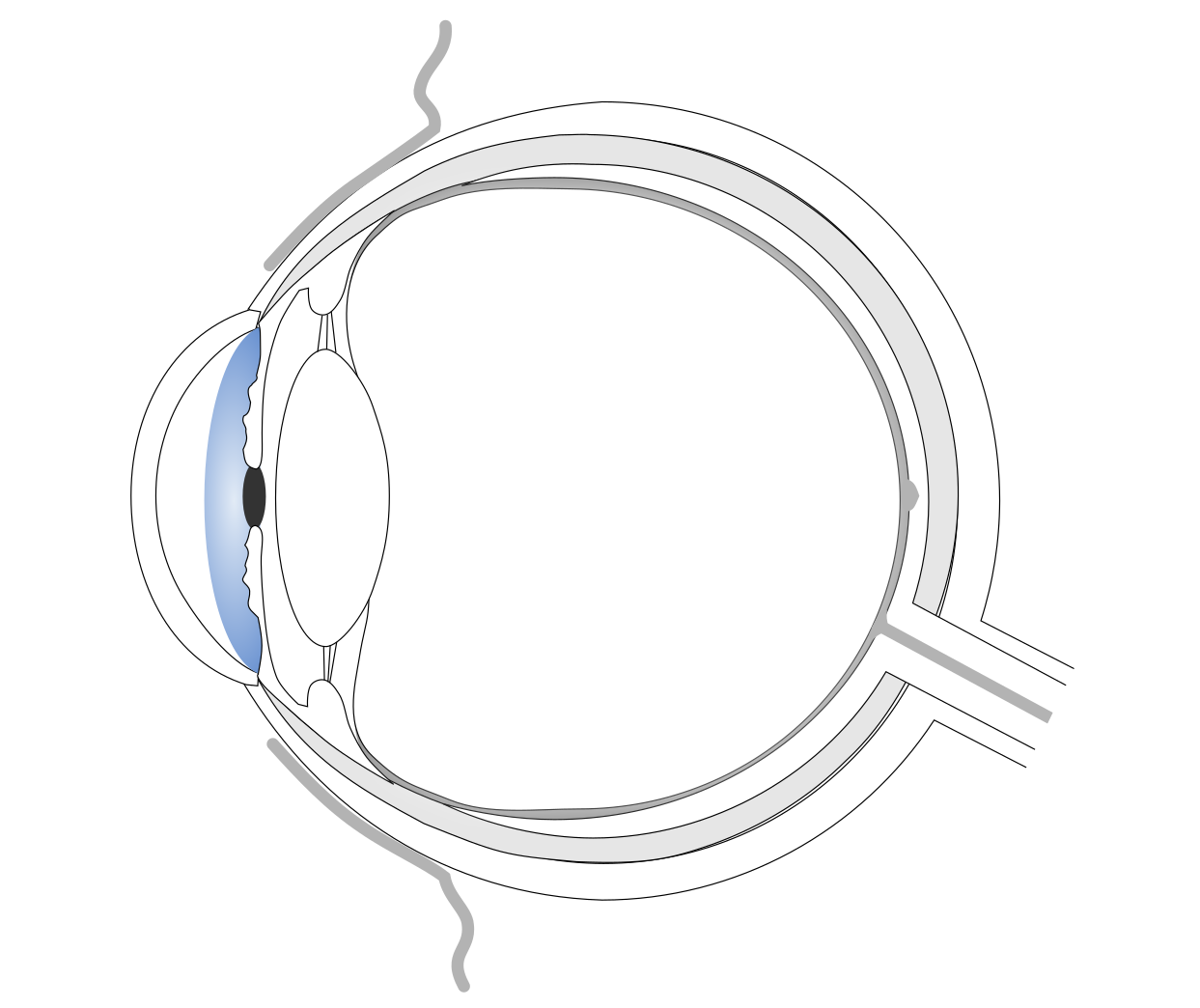
Glaucoma drainage devices (also called shunts) can help to manage intraocular pressure (IOP) in patients with severe uncontrolled glaucoma, who have failed previous glaucoma surgery. The devices consist of a plate and an attached tube. The plate is implanted onto the sclera and the tube is directed into the anterior chamber. Following the surgery, aqueous humor will flow from the anterior chamber into an external reservoir (a fibrous capsule that forms around the plate) to reduce the eye pressure. The devices are mostly made of biocompatible and non-degradable silicone or polypropylene.[8]
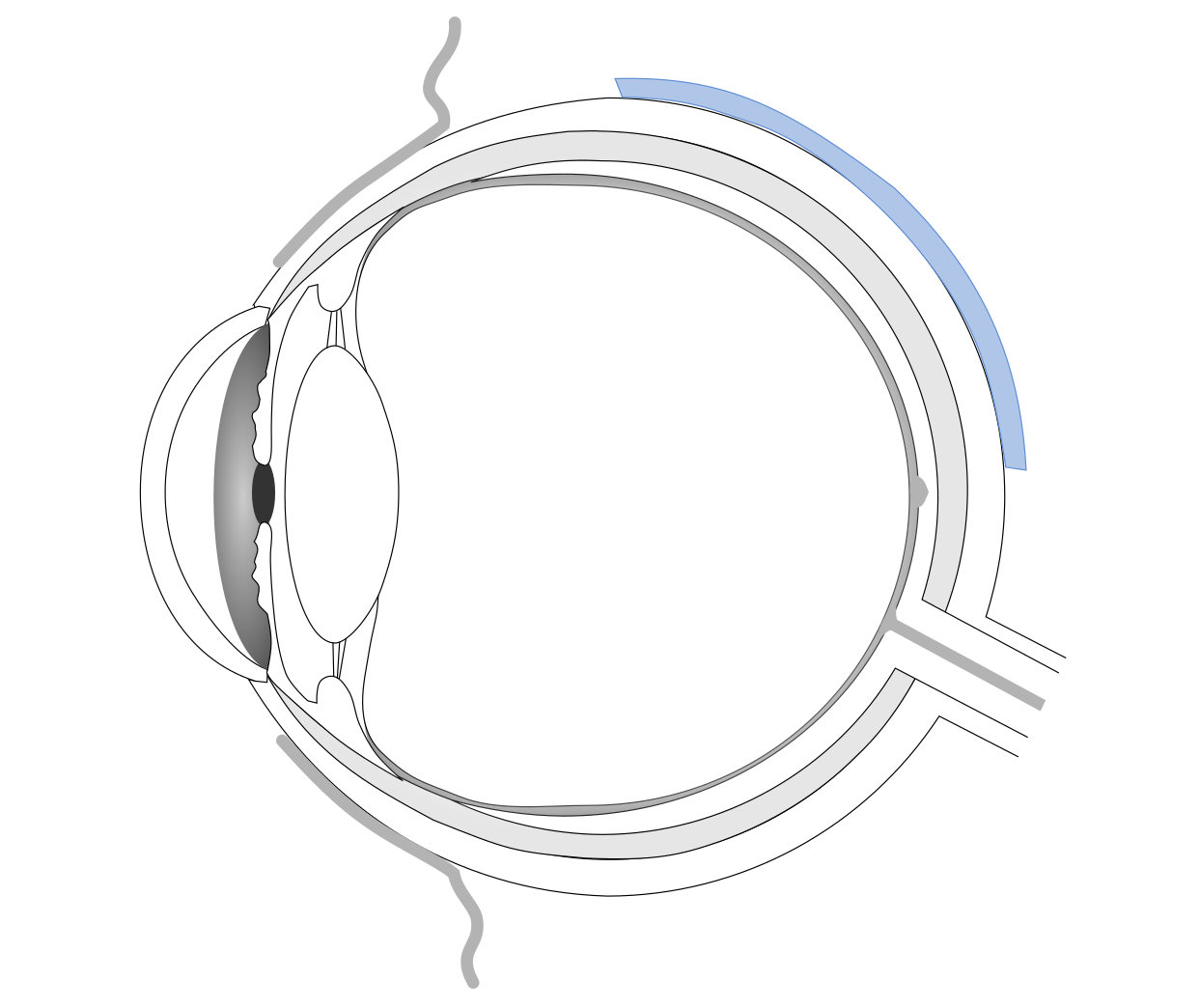
In part 1 of this series, I introduced injectable ocular tamponades as a means to treat retinal detachment. An alternative/complementary treatment involves scleral buckles. Scleral buckles are silicone rubber elements with different shapes from sponges to rubber bands.[9] They are secured to the scleral surface to produce an indent in the eye. This pushes the eye walls closer to the detached retina, so it can re-attach.
Furthermore, tissue adhesives can be applied to seal tears in the retina or to close other wounds in and around the eye, e.g. after cataract surgery.[10] Synthetic adhesives comprise cyanoacrylates, which rapidly polymerize in contact with basic substances, such as water or blood, to form strong bonds. The chemical reaction that takes place generates heat, which might damage the surrounding tissue. Adhesives based on the natural protein fibrin are more biocompatible, but polymerize slowly and yield less strong glues.
Finally, lacrimal plugs are tiny polymer devices that are inserted into the tear duct to block the drainage of tear fluid in patients with chronic dry eyes.[11] The blockage increases the eye’s tear film and surface moisture. The plugs can be semi-permanent, made of e.g. silicone polymer, and have to be removed after some time. Or they can be biodegradable, made from collagen, and dissolve over time.
Conclusion
As you can see, the list of applications for polymers in ophthalmology is long. Part 1 and 2 of this series together should give a comprehensive overview of the topic, but it is likely that I have missed something. If you know of any further eye treatments that involve polymers, please share your knowledge in the comments below!
Polymers are fascinating materials that can have vastly different properties. They are already omnipresent in ophthalmology and other medical disciplines, but they are far from having reached their full potential yet. I’m convinced that the ongoing research in the field will yield exciting new materials and technologies in the future, which will improve the lives of millions of people worldwide. Thanks for coming along on this expedition!
[1] https://www.allaboutvision.com/contacts/contact_lenses.htm, accessed 19.10.2018.
[2] Eurostat, “Surgical operations and procedures statistics”, http://ec.europa.eu/eurostat/statistics-explained/index.php?title=Surgical_operations_and_procedures_statistics, accessed 06.08.2018.
[3] FDA-database search of approved intraocular lenses: https://www.accessdata.fda.gov/scripts/cdrh/devicesatfda/index.cfm?q=aW50cmFvY3VsYXIgbGVucw==&approval_date_from=&approval_date_to=&pagenum=10&sort=approvaldatedesc, accessed 19.10.2018.
[4] https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/PhakicIntraocularLenses/ucm059237.htm, accessed 19.10.2018.
[5] Borja Salvador-Culla & Paraskevi E. Kolovou, “Keratoprosthesis: A Review of Recent Advances in the Field” Journal of Functional Biomaterials, 2016, 7(2), 13. https://doi.org/10.3390/jfb7020013.
[6] Ho Kwon et al., “The Role of Resorbable Plate and Artificial Bone Substitute in Reconstruction of Large Orbital Floor Defect,” BioMed Research International, 2016, Article ID 1358312, 6 pages. https://doi.org/10.1155/2016/1358312.
[7] https://en.wikipedia.org/wiki/Ocular_prosthesis, accessed 22.10.2018.
[8] Sarwat Salim, “Glaucoma Drainage Devices”, American Academy of Ophthalmology – EyeWiki, http://eyewiki.aao.org/Glaucoma_Drainage_Devices, accessed 22.10.2018.
[9] Charles P. Wilkinson, “Scleral buckling for rhegmatogenous retinal detachment”, American Academy of Ophthalmology – EyeWiki, http://eyewiki.aao.org/Scleral_buckling_for_rhegmatogenous_retinal_detachment, accessed 22.10.2018.
[10] Rajesh Sinha et al., “Use of tissue adhesives in ophthalmology”, Indian Journal of Ophthalmology 2009, 57, 409-13. http://www.ijo.in/text.asp?2009/57/5/409/55059.
[11] https://www.allaboutvision.com/conditions/punctal-plugs.htm, accessed 31.10.2018.